Global Healthcare Claims Management Market By Product (Medical Billing, and Claims Processing), By Component (Software, and Services), By Type (Integrated, and Standalone), By Delivery Mode, By End-User, By Region and Companies - Industry Segment Outlook, Market Assessment, Competition Scenario, Trends, and Forecast 2023-2032
- Published date: oct
- Report ID: 67237
- Number of Pages: 286
- Format:
-
keyboard_arrow_up
Quick Navigation
Report Overview
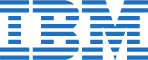
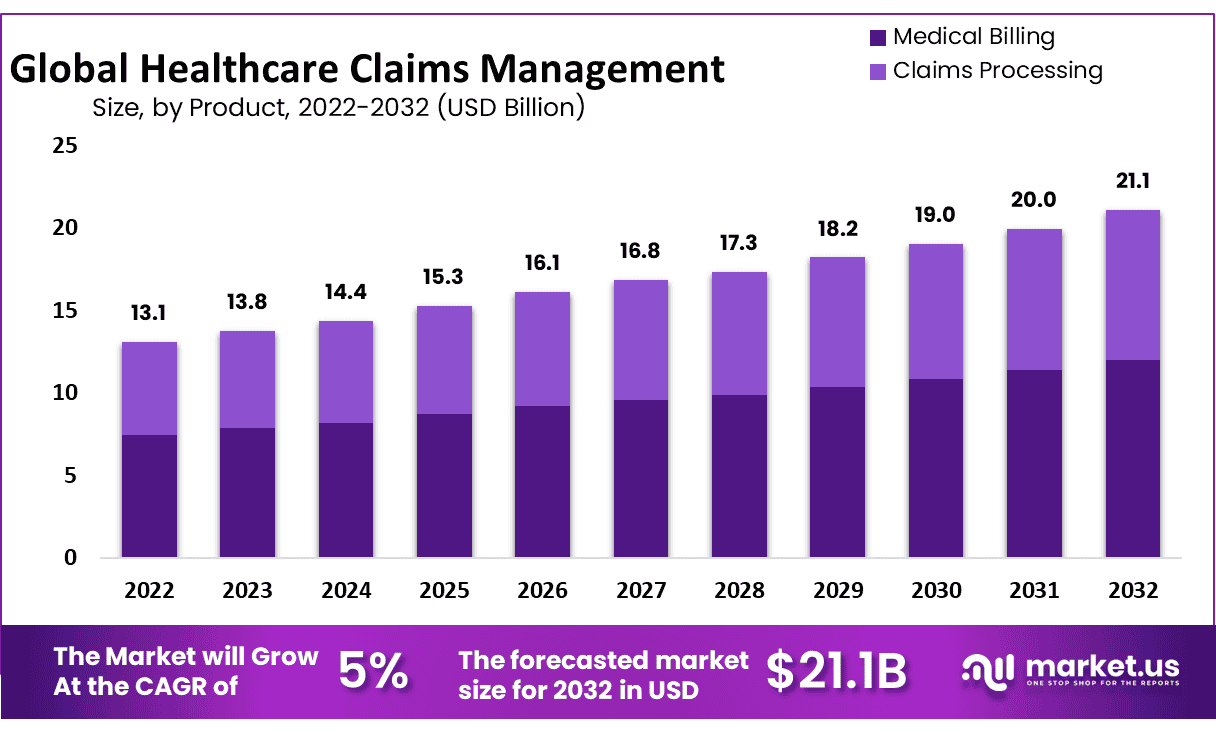
The Global Healthcare Claims Management Market size is expected to be worth around USD 21.1 Billion by 2032 from USD 13.1 Billion in 2022, growing at a CAGR of 5% during the forecast period from 2023 to 2032.
The global healthcare claims management market refers to the market for software and services that manage and process healthcare insurance claims. Healthcare claims management involves the submission, processing, and settlement of medical claims for services rendered by healthcare providers.
The goal of claims management is to ensure that claims are processed accurately and efficiently, which helps to reduce costs and improve the quality of care for patients. The market includes various solutions and services such as claims management software, claim processing and adjudication services, and consulting and outsourcing services for claims management.
The market is driven by factors such as the increasing volume of healthcare claims, the need for efficient claims processing and cost containment, and the growing adoption of electronic health records (EHRs) and healthcare IT solutions.
*Actual Numbers Might Vary In The Final Report
Key Takeaways
- Rising Healthcare Costs: Healthcare claims management market is expanding due to increasing healthcare expenses and demand for efficient claims processing and administration services.
- Increase in Health Insurance Coverage: With increasing health coverage worldwide, both in developed and developing regions alike are demanding simplified claims management processes to handle claims more quickly and efficiently.
- Focus on Cost Containment: Healthcare providers and payers have placed greater importance on cost containment and revenue cycle optimization, making claims management solutions essential.
- Automation and Technology: Technological advances such as artificial intelligence (AI) and machine learning are being leveraged for automating claims processing and improving accuracy.
- Claims Management Systems Can Reduce Administrative Burden: Claims management systems assist healthcare providers by alleviating administrative work so that they can focus more fully on patient care.
- Compliance to healthcare regulations and standards: Compliance is one of the main drivers behind adopting claims management solutions.
Product Analysis
Based on Product, the market for healthcare claims management is segmented into Medical Billing, & Claims. The Medical Billing segment is the most lucrative in the global healthcare claims management market, with a projected CAGR of 5%. The total revenue share of medical billing-type healthcare claims management is 57% in 2022. Claims processing involves the management of insurance claims, including the review, adjudication, and payment of claims submitted by healthcare providers. This includes verifying the accuracy of the claims, determining the covered benefits under the insurance policy, and processing the payment to the healthcare provider.
Both medical billing and claims processing are critical components of healthcare claims management and are typically offered as separate solutions or as part of a larger claims management platform. The growth of the healthcare claims management market is driven by the increasing volume of healthcare claims and the need for more efficient and accurate processing of these claims.
Component Analysis
By Components, the market is further divided into software and services. The software segment is estimated to be the most lucrative segment in the global healthcare claims management market, with a market share of 67% and a projected CAGR of 5%, in 2022. Services for healthcare claims management typically include consulting, outsourcing, and support services.
Consulting services may include assessments of claims management processes and recommendations for improvement, while outsourcing services may involve the outsourcing of claims processing to a third-party service provider. Support services may include training, maintenance, and technical support for software solutions. Both software and services are critical components of healthcare claims management and are often offered together as part of a comprehensive solution for managing healthcare claims.
Type Analysis
Based on type, the market for healthcare claims management is segmented into Integrated, & Standalone. The Integrated segment is the most lucrative in the global healthcare claims management market, with a projected CAGR of 5%. The total revenue share of Integrated-type healthcare claims management is 71% in 2022.
Integrated healthcare claims management solutions are typically part of a larger healthcare IT platform that includes other software solutions such as electronic health records, practice management software, and revenue cycle management (RCM) solutions. Integrated solutions offer greater efficiency and interoperability between different components of the healthcare IT infrastructure.
Delivery Analysis
By Delivery, the market is further divided into, On-Premise, Cloud Based, and Web-Based. The Web-Based segment is estimated to be the most lucrative segment in the global healthcare claims management market, with a market share of 48% and a projected CAGR of 5%, in 2022. On-premise healthcare claims management solutions typically involve software installed and maintained on local servers within a healthcare organization’s IT infrastructure.
Cloud-based healthcare claims management solutions typically involve software that is hosted on remote servers and accessed via the Internet. This solution offers greater flexibility, scalability, and lower upfront costs, as well as the ability to access data from anywhere with an internet connection. Web-based healthcare claims management solutions typically involve software that is accessed through a web browser, often via a subscription-based service.
End-User Analysis
Based on end-user, the market is segmented into healthcare Payers, Healthcare Providers, & Other End-Users. Among these end-users, the healthcare Providers, segment is estimated to be the most lucrative segment in the global healthcare claims management market, with the largest revenue share of 67% and a projected CAGR of 5% during the forecast period.
Healthcare providers, such as hospitals, clinics, and physician practices, are the primary end-users of healthcare claims management solutions. These providers submit claims for services rendered to insurance companies and require efficient and accurate claims processing to receive timely reimbursement.
Key Market Segments
Based on Product
- Medical Billing
- Professional
- Institutional
- Claims Processing
Based on Component
- Software
- Services
Based on Type
- Integrated
- Standalone
Based Delivery Mode
- On-Premise
- Cloud-Based
- Web-based
Based on End-Users
- Healthcare Payers
- Healthcare Providers
- Other End-Users
Drivers
Increasing volume and complexity of healthcare claims
With the rise in healthcare costs and the aging population, the volume and complexity of healthcare claims are increasing. Healthcare claims management solutions help healthcare providers and insurance companies manage these claims more efficiently, reducing costs and improving patient outcomes.
Need for more efficient and accurate processing
Healthcare claims management solutions help streamline the claims management process, reducing errors, and improving accuracy. This leads to faster claim processing and reimbursement, improving overall patient satisfaction.
Growing adoption of electronic health records and healthcare IT solutions
The adoption of EHRs and other healthcare IT solutions is increasing, which is driving the demand for healthcare claims management solutions that integrate with these systems.
Restraints
Concerns over data privacy and security
Healthcare claims management solutions involve the processing and storage of sensitive patient data, which raises concerns over data privacy and security. Healthcare organizations and insurance companies must ensure that they comply with regulations such as the Health Insurance Portability and Accountability Act (HIPAA) and the General Data Protection Regulation (GDPR) to protect patient data.
Complexity of healthcare reimbursement systems
Healthcare reimbursement systems can be complex and vary by country, region, and payer. Healthcare claims management solutions must be able to accommodate these different reimbursement systems, which can be challenging.
In summary, while the global healthcare claims management market is expected to grow, there are several factors that may restrain its growth, including high implementation costs, concerns over data privacy and security, lack of interoperability, resistance to change, and the complexity of healthcare reimbursement systems.
Opportunity
Complexity of healthcare reimbursement systems
Healthcare reimbursement systems can be complex and vary by country, region, and payer. Healthcare claims management solutions must be able to accommodate these different reimbursement systems, which can be challenging.
Concerns over data privacy and security
Healthcare claims management solutions involve the processing and storage of sensitive patient data, which raises concerns over data privacy and security. Healthcare organizations and insurance companies must ensure that they comply with regulations such as the Health Insurance Portability and Accountability Act (HIPAA) and the General Data Protection Regulation (GDPR) to protect patient data.
Trends
The global healthcare claims management market is subject to several trends that are shaping the industry, including:
Increased adoption of cloud-based solutions
The adoption of cloud-based healthcare claims management solutions is increasing due to their flexibility, scalability, and cost-effectiveness. Providers are shifting from on-premise solutions to cloud-based solutions to reduce their IT infrastructure costs.
Focus on patient-centric care
The healthcare industry is moving towards a patient-centric care model, where patients are at the center of their care. Healthcare claims management solutions are being designed to provide patients with greater control over their healthcare costs and access to information.
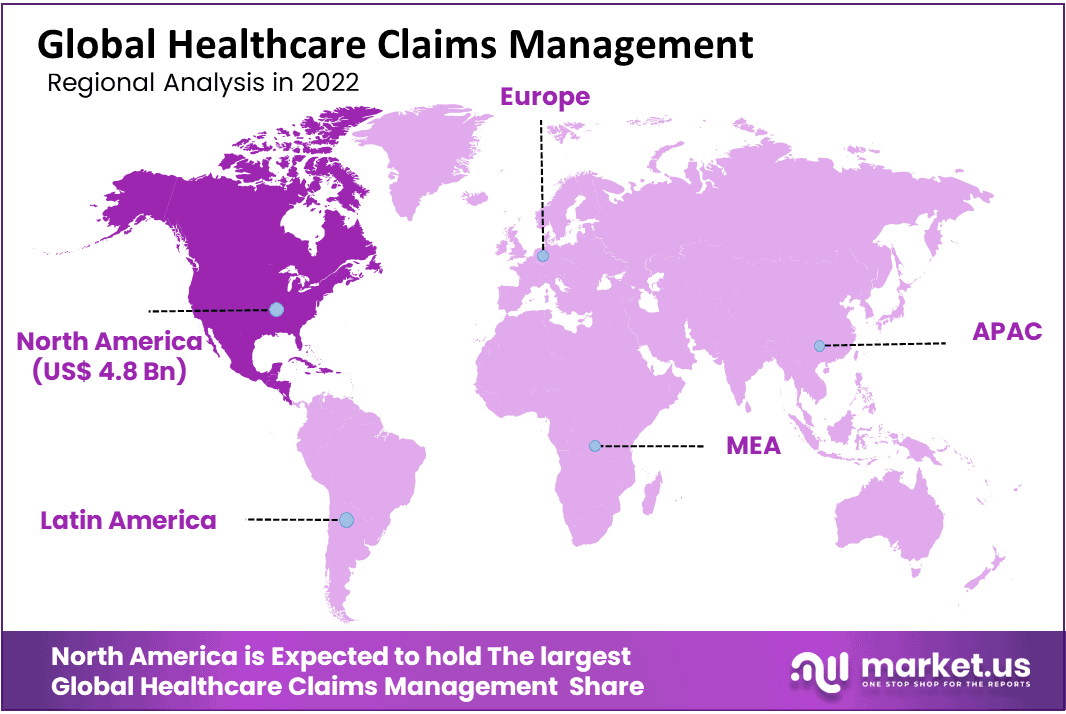
Regional Analysis
North America Generated Highest Revenue Globally and dominated the Global healthcare claims management Market
North America is estimated to be the most lucrative market in the global healthcare claims management market, with the largest market share of 36.8%, and is expected to register a CAGR of 5% during the forecast period. The European healthcare claims management market is expected to grow due to the increasing adoption of healthcare IT solutions and government initiatives to improve healthcare delivery.
The Asia Pacific healthcare claims management market is expected to experience significant growth due to increasing healthcare spending, growing healthcare infrastructure, and government initiatives to digitize healthcare. The Middle East and Africa healthcare claim management market is expected to experience significant growth due to increasing healthcare spending and government initiatives to improve healthcare infrastructure.
Key Regions
- North America
- The US
- Canada
- Mexico
- Western Europe
- Germany
- France
- The UK
- Spain
- Italy
- Portugal
- Ireland
- Austria
- Switzerland
- Benelux
- Nordic
- Rest of Western Europe
- Eastern Europe
- Russia
- Poland
- The Czech Republic
- Greece
- Rest of Eastern Europe
- APAC
- China
- Japan
- South Korea
- India
- Australia & New Zealand
- Indonesia
- Malaysia
- Philippines
- Singapore
- Thailand
- Vietnam
- Rest of APAC
- Latin America
- Brazil
- Colombia
- Chile
- Argentina
- Costa Rica
- Rest of Latin America
- Middle East & Africa
- Algeria
- Egypt
- Israel
- Kuwait
- Nigeria
- Saudi Arabia
- South Africa
- Turkey
- United Arab Emirates
- Rest of MEA
Key Players Analysis
The global healthcare claims management market is highly competitive, and the key players in the market have a significant share of the market. These players have a strong market presence, a wide product portfolio, and a global distribution network. The market is dominated by a few major players, and there are several small and medium-sized players that operate in niche markets. Cerner Corporation, McKesson Corporation, and UnitedHealth Group are the top players in the global healthcare claims management market.
These companies offer a wide range of solutions, including software and services, and have a global presence. They also focus on strategic partnerships, collaborations, and mergers and acquisitions to expand their market share and increase their customer base.
Listed below are some of the most prominent global healthcare claims industry players.
Market Key Players
- Athenahealth
- Plexus Healthcare Systems Inc.
- Cognizant
- Oracle
- Allscripts Healthcare LLC
- nThrive Revenue Systems, LLC
- eClinicalWorks
- Context Healthcare Inc.
- Optum, Inc.
- Mckesson Corporation
- DST Systems
- Ram Technologies Inc.
- General Electric
- Health Solutions Plus (HSP)
- Conifer Health Solutions, LLC
- Quest Diagnostics Incorporated
- Gebbs Healthcare Solutions
- The SSI Group, LLC
- Other Key Players
Recent Developments
- In December 2021, Change Healthcare announced the launch of its Claims Lifecycle AI, a new claims management solution powered by artificial intelligence (AI) and machine learning (ML) technologies.
- In October 2021, McKesson Corporation announced the launch of its new claims management platform, McKesson ClaimsXten Cloud, which is designed to help payers and providers manage their claims more efficiently.
Report Scope
Report Features Description Market Value (2022) USD 13.1 Bn Forecast Revenue (2032) USD 21.1 Bn CAGR (2023-2032) 5% Base Year for Estimation 2022 Historic Period 2016-2022 Forecast Period 2023-2032 Report Coverage Revenue Forecast, Market Dynamics, COVID-19 Impact, Competitive Landscape, Recent Developments Segments Covered By Product-Medical Billing, and Claims Processing; By Component -Software, and Services; By Type -Integrated, and Standalone; By Delivery Mode- On-Premise, Cloud Based, Web-based; By End-User- Healthcare Payers, Healthcare Providers, Other End-Users Regional Analysis North America – The US, Canada, & Mexico; Western Europe – Germany, France, The UK, Spain, Italy, Portugal, Ireland, Austria, Switzerland, Benelux, Nordic, & Rest of Western Europe; Eastern Europe – Russia, Poland, The Czech Republic, Greece, & Rest of Eastern Europe; APAC – China, Japan, South Korea, India, Australia & New Zealand, Indonesia, Malaysia, Philippines, Singapore, Thailand, Vietnam, & Rest of APAC; Latin America – Brazil, Colombia, Chile, Argentina, Costa Rica, & Rest of Latin America; Middle East & Africa – Algeria, Egypt, Israel, Kuwait, Nigeria, Saudi Arabia, South Africa, Turkey, United Arab Emirates, & Rest of MEA Competitive Landscape Athenahealth, Plexus Healthcare Systems Inc., Cognizant, Oracle, Allscripts Healthcare LLC, nThrive Revenue Systems, LLC, eClinicalWorks, Context Healthcare Inc., Optum, Inc., Mckesson Corporation, DST Systems, Ram Technologies Inc., General Electric, Health Solutions Plus (HSP), Conifer Health Solutions, LLC, Quest Diagnostics Incorporated, Gebbs Healthcare Solutions, The SSI Group, LLC, Other Key Players Customization Scope Customization for segments, region/country-level will be provided. Moreover, additional customization can be done based on the requirements. Purchase Options We have three licenses to opt for: Single User License, Multi-User License (Up to 5 Users), Corporate Use License (Unlimited User and Printable PDF) Frequently Asked Questions (FAQ)
What is the Healthcare Claims Management Market?The Healthcare Claims Management Market refers to the industry that focuses on the processing, submission, and management of healthcare insurance claims, including billing, payment, and reimbursement processes.
What are the key factors driving the growth of the Healthcare Claims Management Market?Some key factors driving the growth of the Healthcare Claims Management Market include increasing healthcare expenditure, rising insurance fraud cases, the need for efficient claims processing, advancements in healthcare IT solutions, and government initiatives to streamline healthcare administration.
What are the primary components of healthcare claims management?Healthcare claims management typically involves several components, including claims processing, verification of patient information, coding and documentation, submission of claims to insurance companies, adjudication of claims, payment processing, denial management, and appeals.
How does healthcare claims management benefit healthcare providers?Healthcare claims management helps providers streamline their billing and reimbursement processes, reduce administrative burdens, minimize claim denials and payment delays, improve revenue cycle management, and enhance overall operational efficiency.
What technologies are commonly used in healthcare claims management?Healthcare claims management often relies on advanced technologies such as electronic health records (EHRs), practice management systems, claims processing software, automated coding systems, data analytics, artificial intelligence (AI), and robotic process automation (RPA).
 Healthcare Claims Management MarketPublished date: octadd_shopping_cartBuy Now get_appDownload Sample
Healthcare Claims Management MarketPublished date: octadd_shopping_cartBuy Now get_appDownload Sample -
-
- Athenahealth
- Plexus Healthcare Systems Inc.
- Cognizant
- Oracle
- Allscripts Healthcare LLC
- nThrive Revenue Systems, LLC
- eClinicalWorks
- Context Healthcare Inc.
- Optum, Inc.
- Mckesson Corporation
- DST Systems
- Ram Technologies Inc.
- General Electric
- Health Solutions Plus (HSP)
- Conifer Health Solutions, LLC
- Quest Diagnostics Incorporated
- Gebbs Healthcare Solutions
- The SSI Group, LLC
- Other Key Players