Healthcare Payer Solutions Market By Service Type (Business Process Outsourcing, Knowledge Process Outsourcing, and Information Technology Outsourcing), By Application (Claims Management Services, Member Management Services, Integrated Front Office Service & Back Office Operations, Provider Management Services, Billing & Accounts Management Services, Analytics & Fraud Management Services, Payment Management Services, HR Services, and Audit & Analysis Systems), By End-User (Private Payers and Public Payers), Region and Companies – Industry Segment Outlook, Market Assessment, Competition Scenario, Trends and Forecast 2025-2034
- Published date: May 2025
- Report ID: 149073
- Number of Pages: 306
- Format:
-
keyboard_arrow_up
Quick Navigation
Report Overview
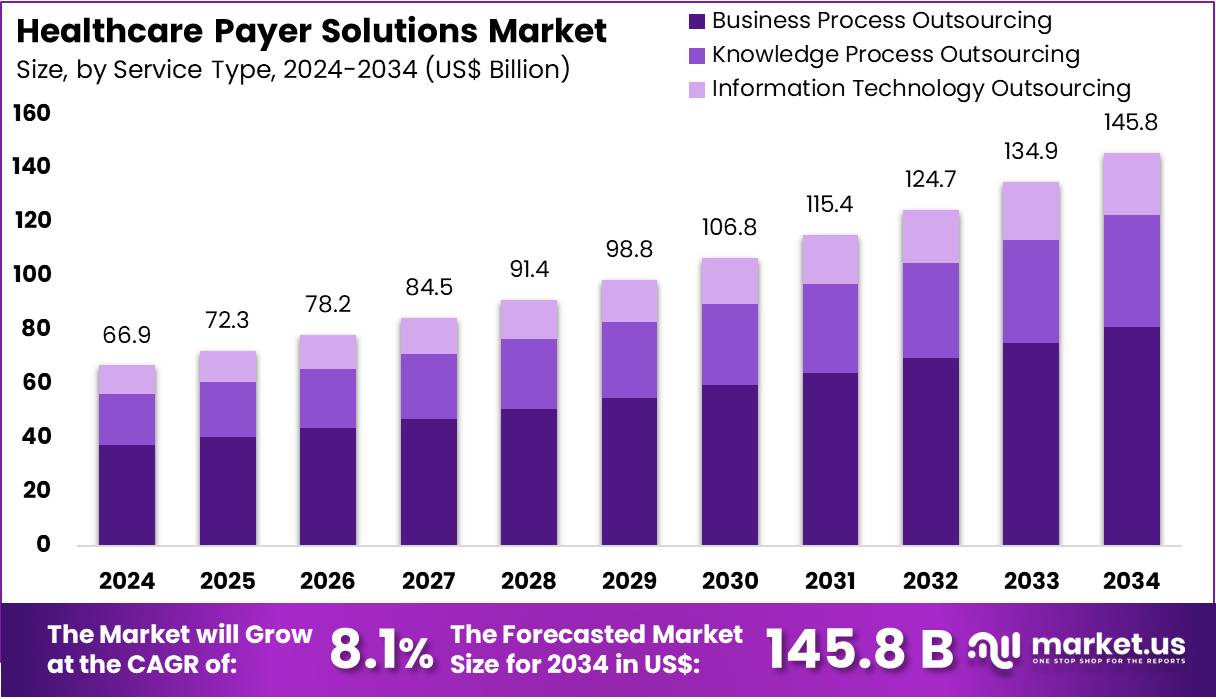
The Healthcare Payer Solutions Market Size is expected to be worth around US$ 145.8 billion by 2034 from US$ 66.9 billion in 2024, growing at a CAGR of 8.1% during the forecast period 2025 to 2034.
Rising demand for efficient healthcare cost management and improved patient outcomes drives the expansion of healthcare payer solutions, which provide critical tools for claims processing, risk adjustment, care coordination, and population health management. These solutions enable payers to analyze vast amounts of healthcare data in real time, enhancing decision-making and operational efficiency.
The launch of IMAT Solutions’ new service in March 2022 highlights advancements in SaaS-based healthcare data management, offering robust clustering capabilities and supporting a diverse range of stakeholders, including payers, statewide organizations, and Health Information Exchanges (HIEs). This service’s NCQA-approved Data Aggregator Validation (DAV) certification emphasizes its reliability and adherence to industry standards.
Healthcare payer solutions also facilitate compliance with regulatory requirements, fraud detection, and provider network management, while enabling value-based care initiatives. The integration of artificial intelligence and advanced analytics further improves risk stratification, member engagement, and predictive modeling. Growing adoption of cloud technologies and interoperability standards opens opportunities for scalable, secure, and cost-effective solutions.
Market trends reveal an increasing focus on personalized health plans, social determinants of health, and patient-centric care models. As payers face evolving challenges in reimbursement and healthcare delivery, payer solutions remain essential in supporting sustainable healthcare ecosystems and enhancing the quality and affordability of care.
Key Takeaways
- In 2024, the market for healthcare payer solutions generated a revenue of US$ 66.9 billion, with a CAGR of 8.1%, and is expected to reach US$ 145.8 billion by the year 2033.
- The service type segment is divided into business process outsourcing, knowledge process outsourcing, and information technology outsourcing, with business process outsourcing taking the lead in 2024 with a market share of 55.7%.
- Considering application, the market is divided into claims management services, member management services, integrated front office service & back office operations, provider management services, billing & accounts management services, analytics & fraud management services, payment management services, hr services, and audit & analysis systems. Among these, claims management services held a significant share of 24.6%.
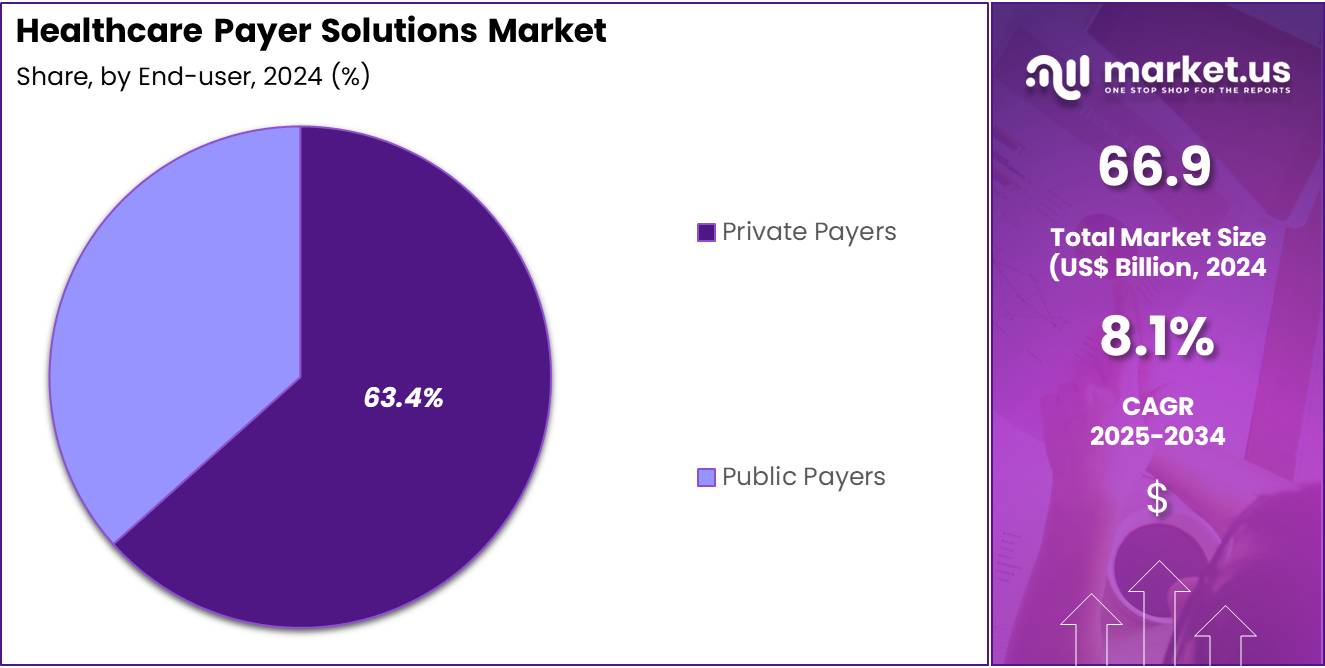
- Furthermore, concerning the end-user segment, the market is segregated into private payers and public payers. The private payers sector stands out as the dominant player, holding the largest revenue share of 63.4% in the healthcare payer solutions market.
- North America led the market by securing a market share of 38.9% in 2024.
Service Type Analysis
The business process outsourcing segment claimed a market share of 55.7% owing to the increasing need for cost-effective operational support. Payers seek to delegate routine administrative tasks such as claims processing, customer service, and data management to specialized third-party providers. This approach allows organizations to focus on core competencies while reducing overhead expenses.
Additionally, the complexity of regulatory compliance and evolving healthcare policies intensifies the demand for expert outsourcing services. Enhanced technological capabilities and automation further enable efficient service delivery by outsourcing firms. Consequently, healthcare payers increasingly rely on business process outsourcing to improve scalability, accuracy, and operational agility, driving significant segment expansion.
Application Analysis
The claims management services held a significant share of 24.6% due to the rising volume and complexity of healthcare claims. Payers require sophisticated solutions to streamline claims adjudication, reduce errors, and minimize fraud. Increasing regulatory scrutiny and the need for faster reimbursement cycles push payers to adopt advanced claims management technologies.
Integration with analytics and fraud detection tools enhances operational efficiency and financial control. Moreover, the shift toward value-based care models emphasizes accuracy and transparency in claims processing. As a result, payers prioritize investments in claims management services to optimize workflows and improve member satisfaction, fueling this segment’s growth.
End-user Analysis
The private payers segment had a tremendous growth rate, with a revenue share of 63.4% owing to the expanding role of private insurance providers in healthcare coverage. Rising healthcare costs and increasing insured populations drive private payers to adopt advanced solutions that improve member engagement, claims processing, and provider network management. Private payers prioritize digital transformation to enhance operational efficiency and customer experience.
Additionally, competitive pressures and regulatory changes encourage private payers to leverage innovative technologies and analytics for better decision-making. This segment benefits from higher adoption rates of customized and scalable solutions, positioning private payers as key growth drivers in the market.
Key Market Segments
By Service Type
- Business Process Outsourcing
- Knowledge Process Outsourcing
- Information Technology Outsourcing
By Application
- Claims Management Services
- Member Management Services
- Integrated Front Office Service & Back Office Operations
- Provider Management Services
- Billing & Accounts Management Services
- Analytics & Fraud Management Services
- Payment Management Services
- HR Services
- Audit & Analysis Systems
By End-User
- Private Payers
- Public Payers
Drivers
Increasing Healthcare Costs is driving the market
The continuous increase in healthcare costs globally is a significant driver for the healthcare payer solutions market. As healthcare expenditures rise, the financial strain on individuals and governments intensifies, thereby increasing the need for effective cost management. In the US, health care spending reached US$ 4.5 trillion in 2022, which accounted for 17.3% of the nation’s GDP, according to the Centers for Medicare & Medicaid Services (CMS).
This substantial portion of the GDP underscores the critical need for solutions that can help manage these escalating costs. Healthcare payers are central to this effort through their management of insurance plans, claims, and utilization. The demand for payer solutions that can navigate the complexities of healthcare financing and reimbursement is therefore growing. These solutions often incorporate technology to enhance efficiency and affordability.
Restraints
Data Security and Privacy Concerns are restraining the market
Despite the increasing demand for efficient healthcare payer solutions, significant concerns about data security and patient privacy can restrain market growth. The healthcare sector manages a large volume of sensitive personal and medical information, making it a target for cyberattacks. Regulations such as HIPAA in the US mandate strict data protection measures.
In 2023, there were 725 reported healthcare data breaches involving 500 or more records reported to the HHS Office for Civil Rights. These breaches compromised the records of over 179 million individuals. Such concerns can impede the adoption of cloud-based and data-sharing solutions crucial for advanced payer technologies. Healthcare payers must heavily invest in security and compliance, which can sometimes slow down the adoption of innovative solutions, thus acting as a restraint on the market.
Opportunities
Rising Adoption of Digital Health Technologies creates growth opportunities
The increasing integration of digital health technologies is creating substantial growth opportunities within the healthcare payer solutions market. These technologies include telehealth, AI, mobile health applications, and wearable devices. The 2021 National Health Interview Survey reported that approximately 37.0% of US adults had used telehealth services in the past 12 months.
Payers can utilize these digital tools to offer more personalized plans, improve patient engagement, and streamline administrative processes like claims. For instance, AI can enhance fraud detection and automate aspects of claims processing. As the healthcare landscape digitizes further, the need for payer solutions capable of leveraging these advancements will continue to expand, fostering market growth.
Impact of Macroeconomic / Geopolitical Factors
Macroeconomic and geopolitical factors significantly affect the healthcare payer solutions market. Economic downturns and inflation can pressure healthcare organizations to seek more efficient solutions, including advanced analytics for cost management. Geopolitical instability can disrupt supply chains for necessary IT infrastructure, potentially raising operational costs for the deployment of payer solutions. Simultaneously, government initiatives aimed at improving healthcare quality and access can spur investment in technology within this market.
For example, legislative measures may incentivize the adoption of digital tools that enhance efficiency. Furthermore, the increasing global focus on data privacy regulations necessitates the integration of robust security features within payer solutions. Consequently, while macroeconomic and geopolitical factors can present challenges like increased costs, they also drive innovation and the need for adaptable and secure healthcare payer solutions.
Current US tariffs are generating a complex set of impacts on the healthcare payer solutions market. Increased tariffs on medical equipment and pharmaceuticals can lead to higher healthcare service costs, which subsequently affect the claims processed by payers. This situation might necessitate adjustments in premium structures. Tariffs on IT infrastructure components could also increase the operational expenses for payer organizations that rely on technology for their solutions.
Despite these potential cost pressures, tariffs could indirectly stimulate demand for solutions that enhance efficiency and reduce operational overhead, such as automation in claims processing and customer service. Moreover, tariffs might encourage a shift towards domestic or regional IT service providers, potentially influencing the vendor landscape within the payer solutions market as organizations seek to mitigate the financial impact of these trade policies.
Latest Trends
Focus on Value-Based Care is a recent trend in the market
A notable recent trend in the healthcare payer solutions market is the growing emphasis on value-based care (VBC) models. These models are shifting the focus from the quantity of services provided to the quality of care and patient outcomes. In 2023, approximately 17.6% of the US GDP was attributed to healthcare spending, a slight increase from 17.4% in 2022, according to the CMS. This context highlights the ongoing efforts to optimize the value derived from this significant expenditure.
The transition to VBC necessitates sophisticated payer solutions that can support the tracking of quality metrics, manage risk, and facilitate new payment models. Payers are increasingly adopting technologies to enable these arrangements, promote preventive care, and improve the management of chronic conditions, driving demand for solutions that support this shift.
Regional Analysis
North America is leading the Healthcare Payer Solutions Market
North America dominated the market with the highest revenue share of 38.9% owing to the need for efficient management of increasing healthcare expenditures. The US saw a 7.5% increase in national health spending in 2023, totaling US$ 4.9 trillion, according to a December 2024 report by CMS. This rise in spending necessitates sophisticated payer solutions for claims processing and financial management. Furthermore, the increasing adoption of value-based care models, with CMS aiming for 100% Medicare beneficiaries in accountable care relationships by 2030, requires advanced analytics and payment systems that these solutions provide.
The Asia Pacific region is expected to experience the highest CAGR during the forecast period
Asia Pacific is expected to grow with the fastest CAGR owing to increasing government efforts to broaden health insurance coverage across the region. For instance, many countries are implementing or expanding universal healthcare programs, leading to a larger pool of insured individuals. This growing insured population necessitates more sophisticated and efficient payer solutions to manage the resulting increase in claims and administrative processes.
Furthermore, a greater emphasis on digitalizing healthcare infrastructure across Asia Pacific is creating opportunities for advanced tech-enabled payer solutions. Payers are also increasingly recognizing the need for solutions that can help detect and prevent fraud, waste, and abuse, which is becoming more prevalent with the expanding healthcare ecosystem.
Key Regions and Countries
- North America
- US
- Canada
- Europe
- Germany
- France
- The UK
- Spain
- Italy
- Russia
- Netherland
- Rest of Europe
- Asia Pacific
- China
- Japan
- South Korea
- India
- Australia
- New Zealand
- Singapore
- Thailand
- Vietnam
- Rest of APAC
- Latin America
- Brazil
- Mexico
- Rest of Latin America
- Middle East & Africa
- South Africa
- Saudi Arabia
- UAE
- Rest of MEA
Key Players Analysis
Key players in the healthcare payer solutions market focus on strategies such as digital transformation, strategic acquisitions, and the integration of advanced technologies to drive growth. They prioritize enhancing operational efficiency through automation and data analytics, aiming to improve claims processing and fraud detection.
Companies also emphasize expanding their service portfolios to include value-based care models and personalized member engagement solutions. Furthermore, they invest in cybersecurity measures to protect sensitive health information and comply with regulatory requirements. Collaborations with technology providers enable the development of scalable and interoperable platforms that meet the evolving needs of healthcare payers.
UnitedHealth Group, a prominent player in this sector, operates through its technology and services division, Optum. Optum offers a comprehensive suite of solutions, including OptumInsight, which provides data analytics and technology services to healthcare organizations, and OptumRx, a pharmacy care services business.
In 2022, Optum merged with Change Healthcare, a move aimed at enhancing its capabilities in healthcare technology and payer services. The company continues to expand its footprint through strategic acquisitions, such as the purchase of LHC Group in 2022, to diversify its service offerings and strengthen its position in the healthcare market. Headquartered in Eden Prairie, Minnesota, UnitedHealth Group serves millions of members worldwide, focusing on improving healthcare delivery and outcomes.
Top Key Players in the Healthcare Payer Solutions Market
- CRISPR Therapeutics
- Editas Medicine
- Intellia Therapeutics
- Beam Therapeutics
- Caribou Biosciences
- Mammoth Biosciences
- Synthego
- Thermo Fisher Scientific
Recent Developments
- In September 2023, Genpact deepened its partnership with Amazon Web Services (AWS) to advance financial crime risk operations by utilizing generative AI and large language models. This collaboration aims to create a competitive edge, applying cutting-edge technology to improve risk management and efficiency in the financial sector.
- In April 2023, Cognizant expanded its alliance with Microsoft within the healthcare sector, providing healthcare payers and providers with rapid access to innovative technological solutions. This extended partnership focuses on streamlining claims processing, enhancing interoperability, and improving patient and member experiences, ultimately optimizing business operations in healthcare.
Report Scope
Report Features Description Market Value (2024) US$ 66.9 billion Forecast Revenue (2034) US$ 145.8 billion CAGR (2025-2034) 8.1% Base Year for Estimation 2024 Historic Period 2020-2023 Forecast Period 2025-2034 Report Coverage Revenue Forecast, Market Dynamics, COVID-19 Impact, Competitive Landscape, Recent Developments Segments Covered By Service Type (Business Process Outsourcing, Knowledge Process Outsourcing, and Information Technology Outsourcing), By Application (Claims Management Services, Member Management Services, Integrated Front Office Service & Back Office Operations, Provider Management Services, Billing & Accounts Management Services, Analytics & Fraud Management Services, Payment Management Services, HR Services, and Audit & Analysis Systems), By End-User (Private Payers and Public Payers) Regional Analysis North America – US, Canada; Europe – Germany, France, The UK, Spain, Italy, Russia, Netherlands, Rest of Europe; Asia Pacific – China, Japan, South Korea, India, Australia, New Zealand, Singapore, Thailand, Vietnam, Rest of APAC; Latin America – Brazil, Mexico, Rest of Latin America; Middle East & Africa – South Africa, Saudi Arabia, UAE, Rest of MEA Competitive Landscape CRISPR Therapeutics, Editas Medicine, Intellia Therapeutics, Beam Therapeutics, Caribou Biosciences, Mammoth Biosciences, Synthego, Thermo Fisher Scientific. Customization Scope Customization for segments, region/country-level will be provided. Moreover, additional customization can be done based on the requirements. Purchase Options We have three licenses to opt for: Single User License, Multi-User License (Up to 5 Users), Corporate Use License (Unlimited User and Printable PDF)  Healthcare Payer Solutions MarketPublished date: May 2025add_shopping_cartBuy Now get_appDownload Sample
Healthcare Payer Solutions MarketPublished date: May 2025add_shopping_cartBuy Now get_appDownload Sample -
-
- CRISPR Therapeutics
- Editas Medicine
- Intellia Therapeutics
- Beam Therapeutics
- Caribou Biosciences
- Mammoth Biosciences
- Synthego
- Thermo Fisher Scientific